
Mission
Noora Health’s mission is to improve outcomes and save lives of at-risk patients by empowering family caregivers with the skills they need to care for their loved ones.
Life Challenges of the Women Served
 Nearly one-million children under the age of 5 die in India every year – an estimated 70 percent of which could have been prevented at home. India has made slow progress with respect to child mortality compared to other countries in the region: it ranks 48th out of 89 on infant mortality rate. India contributes more than any other country to newborn death, and it accounts for approximately one-fifth of maternal deaths worldwide. Neonatal mortality contributes to more than one-half of under-five mortality (58 percent) with India reporting 640,000 newborn deaths annually.
Nearly one-million children under the age of 5 die in India every year – an estimated 70 percent of which could have been prevented at home. India has made slow progress with respect to child mortality compared to other countries in the region: it ranks 48th out of 89 on infant mortality rate. India contributes more than any other country to newborn death, and it accounts for approximately one-fifth of maternal deaths worldwide. Neonatal mortality contributes to more than one-half of under-five mortality (58 percent) with India reporting 640,000 newborn deaths annually.
Twenty-seven percent of India’s population lives in poverty, with 21 percent living on less than $1.90 a day. For countless poor families across the country, preventable health complications and deaths occur due to a lack of specific knowledge and inadequate resources to meet their health needs. Public health facilities, where poor people seek healthcare services, have disproportionately far less resources than their private counterparts. They are simply too overstretched and understaffed to meet the demands of the burgeoning population. Patients often travel miles from remote areas, then wait hours just to speak to their healthcare provider. Even after a long wait, the average time that a doctor interacts with a patient in a public health facility in India is less than 2.5 minutes.
On a national level, India’s government expenditure on public healthcare is still only 1.28 percent as a proportion of GDP – this has barely increased in the last 20 years. As a result, the quality of health care in India is affected by a critical shortage in human resources, wherein only 3 million skilled healthcare professionals are available to serve a population of 1.25 billion, or only 24.1 per 10,000 people. The shortage of trained medical professionals in India means that most patients recovering from medical interventions often rely on care provided by family members.
 Most families in these contexts have low health literacy and hold varied beliefs about healthy behaviors, inadvertently leading to poor health outcomes. Anxious patients return to their homes with little understanding of their health conditions, and their families are uncertain of how to care for their loved ones – often leading to post-discharge complications or even deaths.
Most families in these contexts have low health literacy and hold varied beliefs about healthy behaviors, inadvertently leading to poor health outcomes. Anxious patients return to their homes with little understanding of their health conditions, and their families are uncertain of how to care for their loved ones – often leading to post-discharge complications or even deaths.
In families across low resource settings, preventable maternal and newborn complications and deaths occur in the postnatal period due to inadequate health-seeking behaviors. Key risk factors for newborn death include infection, hypothermia, lack of breastfeeding, and failure to recognize warning signs of newborn illness. Often when a complication occurs, it may not be recognized until a much later stage when the situation is far more serious.
The Project
The child mortality risk factors stated above can be combated by practicing essential newborn care behaviors that are shown to reduce newborn complications and mortality. This project aims to reduce the incidence of preventable, newborn complications and deaths. In India, family-oriented structured training programs can address gaps in healthcare created by lack of continuity of care, healthcare workers shortage, and overcrowded government district hospitals. The trained nurses deliver the Care Companion Program in hospital wards and utilize Noora Health’s medically-informed, contextualized interactive videos, flip-charts and handouts to teach essential newborn and maternal care to mothers and family members who are key decision-makers (e.g. grandmothers, mother-in-laws, fathers) in a group class for ~40 minutes before hospital discharge. Noora’s MCH curriculum focuses on behaviors that are proven by research to address mortality and morbidity in mothers and newborns. The content promotes healthy behaviors, proper nutrition, infection control, routine checkups, vaccinations, health seeking behaviors for complications among other health information.
Noora Health will train new mothers and family members how to improve health outcomes through exclusive breastfeeding, skin-to-skin thermal care, hand hygiene, umbilical cord care, postpartum maternal diet, and health-seeking behaviors in response to warning signs among newborn care.

Noora Health’s Care Companion Program (CCP) turns hallways and waiting rooms in public healthcare facilities into classrooms, where hospital staff trained by Noora Health deliver appropriate and relevant health information and training. The goal of this project is to scale Noora Health’s existing CCP across India to achieve the goal of training over 1.1 million new mothers and their families cumulatively by the end of 2021. New mothers and their caregivers in Indian context (mothers, grandmothers, mothers-in-law) are Noora Health’s default target population for the program.
Noora Health conducts in-depth research and needs-finding among their target population. They develop and design materials that take complicated medical information about key health-promoting behaviors and transform it into engaging curriculum, videos, printed materials, and tools that are highly visual and culturally relevant. Content is available in multiple regional languages, and materials are designed for ease of communication, particular in low literacy environments.
Noora Health upskills existing staff in the Government District Hospitals and equips them with the materials, training, and tools they need to confidently conduct the CCP in their facilities. Once the nurses and counselors are trained to deliver the CCP, they train other frontline workers in their hospital facilities to execute the program. The CCP is delivered to families in group settings during their hospital stay, when evidence suggests families are primed to receive and initiate health behavior change.
 The Noora Health Team provides the guidance necessary for successful integration within the care delivery framework. They take a hands-on approach to ensure the smooth transition of the program into the hospital’s daily activities so that family members can learn high-impact, hands-on skills from the trained educators. They also incorporate trainers into their community of educators across India with whom they conduct regular sessions to improve the trainers’ skills and share best practices.
The Noora Health Team provides the guidance necessary for successful integration within the care delivery framework. They take a hands-on approach to ensure the smooth transition of the program into the hospital’s daily activities so that family members can learn high-impact, hands-on skills from the trained educators. They also incorporate trainers into their community of educators across India with whom they conduct regular sessions to improve the trainers’ skills and share best practices.
The CCP supports families throughout their entire healthcare journey beyond the confines of the hospital. Families can also opt-in to Noora’s WhatsApp engagement service, which allows for two-way communication with qualified medical practitioners. Caregivers and patients ask questions and receive tailored support, which serves as a vital and personalized link in situations where accessing a doctor or hospital is challenging. This allows for a continuity of care that is otherwise absent for patient populations in these geographies. Evidence suggests that combining pre-discharge education with post-discharge follow-up can be an effective mechanism to improve health outcomes.
Noora Health has been able to leverage WhatsApp for COVID-19, at a time when the focus on family and caregiver training is even more important, especially in relation to ensuring appropriate care seeking behavior and addressing needs arising out of home-based quarantine, recovery, and prevention for those who need it most. People and healthcare workers are not able to find relevant COVID-19 information due to multiple competing, often inaccurate, messages. Government health advisories are complex and are not being shared effectively. Noora Health is using the WhatsApp technology to bridge this divide by delivering high quality and accurate COVID-19 health content to those who need it the most, remotely engaging them with timely access at crucial moments.
 Direct Impact: Noora Health’s CCP directly impacts mothers, their family members, and in turn their newborn babies. They aim to train 1.1 million mothers and family members by 2021. The project also directly impacts hospital staff in public healthcare facilities who are upskilled and trained to deliver the CCP health information to families. This grant will enable Noora Health to directly train ~90 nurses in the states of Karnataka, Punjab and Maharashtra. These master trainers will then go on to train ~500 nurses and counsellors in the healthcare facilities in which they work.
Direct Impact: Noora Health’s CCP directly impacts mothers, their family members, and in turn their newborn babies. They aim to train 1.1 million mothers and family members by 2021. The project also directly impacts hospital staff in public healthcare facilities who are upskilled and trained to deliver the CCP health information to families. This grant will enable Noora Health to directly train ~90 nurses in the states of Karnataka, Punjab and Maharashtra. These master trainers will then go on to train ~500 nurses and counsellors in the healthcare facilities in which they work.
Indirect Impact: Noora Health’s work will indirectly impact government and hospital stakeholders who support and manage the overburdened healthcare system in India. They are actively working in 159 facilities and by the end of 2021, Noora Health will work with these stakeholders and amplify their work across 225 facilities. In addition, their work will indirectly impact the communities of the patients and family members who are trained by Noora Health’s CCP.
UN Sustainable Development Goals
![]()
Questions for Discussion
- How do you think this project can impact poor communities?
- How do you think empowering caregivers can affect gender equality?
- How could this framework be utilized in other areas of the world?
How the Grant Will be Used
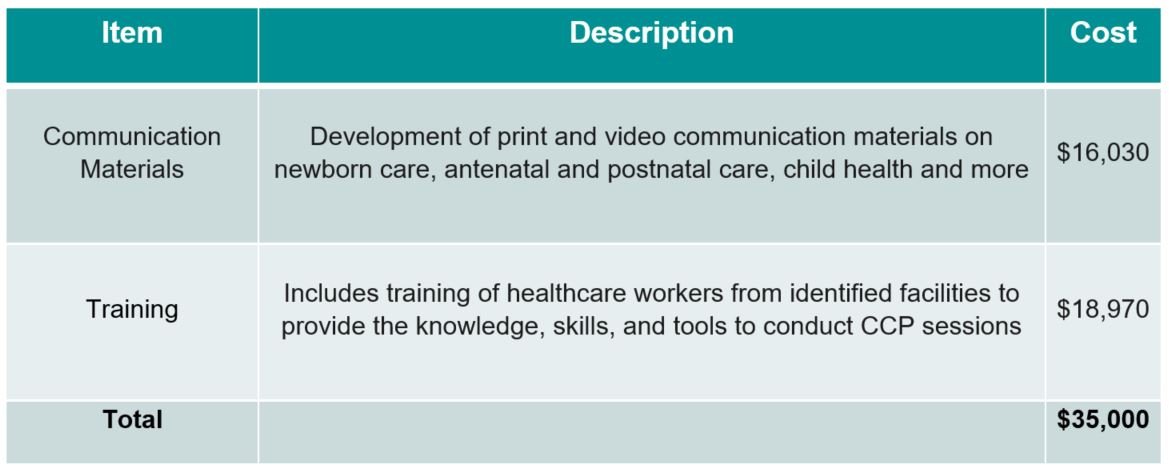
Together Women Rise’s grant of $35,000 will be allocated to direct program expenses to fund two core activities:
Why We Love This Project/Organization
Noora Health excels in strengthening health care services, advocating for policy change, and strengthening provider capacities in low resource settings. Noora Health’s Companion Care Program capitalizes on the untapped potential of extended family members to provide post discharge care that maximizes health outcomes. Noora Health’s model is sustainable, allows for the continuity of care, and enables institutions to build capacity over time and better serve their constituents.
Evidence of Success
 To date, Noora Health has trained more than 770,000 patients and family members across 159 facilities. CCP has been proven to demonstrate a 71 percent decrease in post-surgical complications, an 18 percent decrease in neonatal complications, a 23 percent reduction in surgical readmissions, a 42 percent reduction in neonatal inpatient readmissions, and a 27 percent increase in outpatient visits. The pilot and ongoing studies are proving the uptake of healthy behaviors, an improvement in overall quality of life (WHO-Quality of Life measure), and an overall increase in the number of highly satisfied patients by 40 percent. In addition, Noora Health has trained more than 3,800 hospital staff pre-COVID and approximately 400 more frontline workers with their COVID-19 work (to-date).
To date, Noora Health has trained more than 770,000 patients and family members across 159 facilities. CCP has been proven to demonstrate a 71 percent decrease in post-surgical complications, an 18 percent decrease in neonatal complications, a 23 percent reduction in surgical readmissions, a 42 percent reduction in neonatal inpatient readmissions, and a 27 percent increase in outpatient visits. The pilot and ongoing studies are proving the uptake of healthy behaviors, an improvement in overall quality of life (WHO-Quality of Life measure), and an overall increase in the number of highly satisfied patients by 40 percent. In addition, Noora Health has trained more than 3,800 hospital staff pre-COVID and approximately 400 more frontline workers with their COVID-19 work (to-date).
Voices of the Girls
“Conducting the CCP has become a part of my daily work routine. I can see the difference in patients’ behavior, especially when engaged attendees ask questions.”
– Nurse Manjula, Care Companion Program Trainer
“As a trainer, I instruct thousands of new mothers and their families on antenatal and postnatal care practices. I’ve formed relationships with so many families, and got so much joy out of spending time with their babies. My goal is to save as many babies’ lives as possible.”
– Nurse Shanthi, Care Companion Program Trainer
“When I came back home, there was nobody to help me or tell me when my breast milk would start. I would ask the team for support on WhatsApp and get quick responses. I followed their advice religiously and Ishaan is healthy and happy.”
– Taslima
“This is my first time hearing about skin-to-skin contact between mother and child and exclusive breastfeeding. It is all new to me, but I am happy that my daughter-in-law has this support, and is learning about the best way to care for her child.”
– Savita
 “I am here since it’s my daughter’s first pregnancy and I was told this class will teach us better care and management. Men, especially husbands, were not involved in the process during our time. It’s good to see that changing.”
“I am here since it’s my daughter’s first pregnancy and I was told this class will teach us better care and management. Men, especially husbands, were not involved in the process during our time. It’s good to see that changing.”
– Rojamma
“This program gave me the confidence to handle my pregnancy and baby. We were taught everything about my diet, breastfeeding, nutrition, cord care and even the importance of immunization for children.”
– Gurpreet Kaur
“After attending these classes, I wonder if my earlier practices might have had an impact on my children – maybe that’s why they also fell sick often? This time I will make sure that I do everything right for this baby so that he doesn’t face any issues.”
– Rekha
About the Organization
 Noora Health was established in 2014 by four graduate students at Stanford in the d. School course “Design for Extreme Affordability.” They traveled to India and found an incredible resource in motivated, compassionate, but untapped caregivers, and a desperate need for higher quality care. What started as a class project soon turned into an obsession, primarily because a simple solution for a direct, tangible need was found. In 2015, they launched their first public hospital partnership with Sri Jayadeva Institute, the largest government cardiac center in South India, and partnered with the private Manipal Hospital chain. In 2016, they launched an oncology training program, and a maternal and newborn care program. In 2018, they piloted a mobile engagement platform on WhatsApp, enabling them to reach patients and families with critical information once they returned home.
Noora Health was established in 2014 by four graduate students at Stanford in the d. School course “Design for Extreme Affordability.” They traveled to India and found an incredible resource in motivated, compassionate, but untapped caregivers, and a desperate need for higher quality care. What started as a class project soon turned into an obsession, primarily because a simple solution for a direct, tangible need was found. In 2015, they launched their first public hospital partnership with Sri Jayadeva Institute, the largest government cardiac center in South India, and partnered with the private Manipal Hospital chain. In 2016, they launched an oncology training program, and a maternal and newborn care program. In 2018, they piloted a mobile engagement platform on WhatsApp, enabling them to reach patients and families with critical information once they returned home.
Noora Health was on Fast Company’s 2016 list of Top 50 Most Innovative Companies in the World (and made the top 10 list for India in 2016 and 2017), and has been supported by TedX, Forbes, Ashoka, Washington Post, Huffington Post, World Health Organization (SIHI) and many large philanthropic foundations. Their program was selected by the Government of India’s Ministry of Health as a Best Practice in both Maternal and Newborn, and Health Systems Strengthening during the National Summit on Innovations in Public Health.
Where They Work


India is in Southern Asia, bordering the Arabian Sea and the Bay of Bengal, between Pakistan and Burma, in an area sized slightly more than one-third the size of the United States. The terrain consists of upland plain (Deccan Plateau) in the south, flat to rolling plain along the Ganges, deserts in the west, and the Himalaya mountains in the north. Natural hazards include droughts, flash floods (as well as widespread and destructive flooding from monsoonal rains), severe thunderstorms, and earthquakes.
 India’s population is more than 1.3 billion (July 2021 est.). There is a very high population density throughout most of the country, with the core of the population in the north along the banks of the Ganges. The median age is 28.7 years. The birth rate is 17.53 births/1,000 population (2021 est.), and the death rate is 7.1 deaths/1,000 population (2021 est.). Life expectancy for the total population is 70 years.
India’s population is more than 1.3 billion (July 2021 est.). There is a very high population density throughout most of the country, with the core of the population in the north along the banks of the Ganges. The median age is 28.7 years. The birth rate is 17.53 births/1,000 population (2021 est.), and the death rate is 7.1 deaths/1,000 population (2021 est.). Life expectancy for the total population is 70 years.
Twenty-two percent of India’s population lives under the poverty line. The maternal mortality rate is 145 deaths/100,000 live births (2017 est.). The infant mortality rate is 39.55 deaths/1,000 live births. Thirty-three percent of children under the age of 5 are underweight (2016/18).
The literacy rate for the total population is 74 percent, with 83 percent of males being able to read, and 66 percent of females (2018). The country’s education expenditures are 3.8 percent of the GDP (2013)
Current environmental issues include deforestation, soil erosion, overgrazing, desertification, air pollution from industrial effluents and vehicle emissions, water pollution from raw sewage and runoff of agricultural pesticides, preservation and quality of forests, and biodiversity loss. Tap water is not potable throughout the country, and the huge and growing population is overstraining the natural resources.
A Closer Look at the Benefits of Engaging Patients and Family Members in Healthcare
Informed patients actively engaged in their healthcare can reduce healthcare costs and improve the quality of outcomes. Moreover, patients often receive care from family caregivers, relatives, friends, and neighbors who are vital to the patient throughout the care and recovery experience.
 Unfortunately, patients, their families and other caregivers, and the public are all too often not meaningfully engaged in healthcare or as partners in its improvement. The lack of patient focus in the healthcare system is also evident in patient transitions between care settings. Patients often report that care transitions, such as being discharged from the hospital, are abrupt. Patients often receive little information about what the next steps are in their care, when they can resume activities, what side effects or complications they should monitor, etc. In other cases, patients receive too much information at the time of discharge, stressing their ability to remember and apply this information over the transition period.
Unfortunately, patients, their families and other caregivers, and the public are all too often not meaningfully engaged in healthcare or as partners in its improvement. The lack of patient focus in the healthcare system is also evident in patient transitions between care settings. Patients often report that care transitions, such as being discharged from the hospital, are abrupt. Patients often receive little information about what the next steps are in their care, when they can resume activities, what side effects or complications they should monitor, etc. In other cases, patients receive too much information at the time of discharge, stressing their ability to remember and apply this information over the transition period.
Patient and family-centered care involves healthcare workers collaborating with patients and families at all levels of healthcare. Patient and family engagement is an important component of patient- and family-centered care. It creates an environment where patients, families, clinicians, and hospital staff all work together as partners. It involves patients and family members as integral members of the healthcare teams from the patient standpoint, and also as advisors working with medical personnel to improve policies and procedures – creating information highways to improve overall quality of care.
Source Materials
