Mission
The mission of the Peter C. Alderman Foundation is to heal the emotional wounds of survivors of terrorism, torture and mass violence by training indigenous health workers and establishing trauma treatment systems in post-conflict countries around the globe.
Life Challenges of the Women Served
In northern Uganda, previous war trauma combines with ongoing poverty, stigma and gender-based violence to form a toxic environment for maternal mental health. The invisible wounds of war – including depression, anxiety, and PTSD – produce enormous suffering and keep as many as one out of four childbearing women from functioning as individuals, mothers, and productive community members. It is estimated that as many as 25 percent of new mothers in the post-conflict setting suffer from postpartum depression. They have increased risk of obstetric complications, preterm labor and suicide. The consequences for their babies are dire, with well-documented evidence that perinatal depression is associated with pre-term birth, low birth weight, increased prevalence of diarrhea, malnutrition, and childhood disease and incomplete immunization schedules.
The mental health treatment gap in conflict-affected African countries exceeds 90 percent. Perinatal depression and anxiety, which are under-recognized and under-treated in the developed world, receive virtually no attention in northern Uganda.
More than 24 percent of PCAF patients in Uganda have had no formal education, and 55 percent have completed only primary education. Nearly 68 percent of patients work in farming or animal husbandry and 11 percent of patients are unemployed. As many as 25 percent of patients report that they are HIV-positive. More than half of PCAF’s patients under the age of 18 are orphans. Conflict and insecurity has been a powerful and long-term driver of chronic poverty in Northern Uganda, with many of the barriers to poverty exit remaining even now after years of peace. Households are more likely to be widow-led, contain a disabled person or orphan, be “gap generation households,” have lower levels of education and be more likely to rely on subsistence agriculture.
The Project
 The program is a stepped-care model that will bring psychosocial and mental health care from PCAF’s hospital-based clinics into the community through increasing the skill levels of community health workers (CHWs), nurses and midwives at northern Uganda’s lower-level health centers. It will be implemented at PCAF’s four multi-disciplinary mental health teams in Soroti, Arua, Gulu and Kitgum. Using its existing clinic and community outreach platform, PCAF will train CHWs, nurses and midwives in providing psychoeducation, basic stress management techniques and how to screen and refer for signs of maternal depression and other forms of mental health problems. PCAF will bring this intervention to scale at Soroti District Hospital and its outreach areas in 2015 and then roll it out to PCAF’s other three northern Uganda clinics. The project will continue implementation with ongoing improvements as needed throughout 2016 and into May 2017.
The program is a stepped-care model that will bring psychosocial and mental health care from PCAF’s hospital-based clinics into the community through increasing the skill levels of community health workers (CHWs), nurses and midwives at northern Uganda’s lower-level health centers. It will be implemented at PCAF’s four multi-disciplinary mental health teams in Soroti, Arua, Gulu and Kitgum. Using its existing clinic and community outreach platform, PCAF will train CHWs, nurses and midwives in providing psychoeducation, basic stress management techniques and how to screen and refer for signs of maternal depression and other forms of mental health problems. PCAF will bring this intervention to scale at Soroti District Hospital and its outreach areas in 2015 and then roll it out to PCAF’s other three northern Uganda clinics. The project will continue implementation with ongoing improvements as needed throughout 2016 and into May 2017.
The CHWs and midwives will screen and monitor pregnant women and new mothers for signs of mental distress. For those women showing signs of mental distress, they will provide workshops in basic self-care, psycho-education and stress management techniques. Women with initial high levels of symptoms and those not improving through stress management will be referred to PCAF specialized professional staff for group therapy, individual counseling and psychiatric intervention, if needed. Mothers and their babies will be followed from the second trimester of pregnancy and continuing, as possible, into the child’s second year of life.
Working directly with pregnant women in the health centers and during community outreaches, the CHWs and midwives will provide screening, psychoeducation, stress management techniques and referrals. PCAF’s community social workers will supervise the CHWs and the midwives on a daily basis. The Project Manager will supervise their work. The Director of Research oversees the collection and analysis of patient data. The social workers at the clinics will provide supervision to the community social workers in kind. All PCAF clinic staff will be available for ongoing patient treatment, as needed. Each of the PCAF clinics is run by a team leader and is supervised by a psychiatrist. The supervising psychiatrists also visit the community outreach sites. PCAF’s Program Director provides overall program supervision. The Uganda Program Director and Deputy Director provide supervision of the outreach program, visit the clinics quarterly and are in regular contact with the clinic team leaders.
Pregnant women and new mothers will be recruited throughout the community, at PCAF outreach and clinic sites, and at the health centers and hospitals where they go for prenatal care. After screening for signs of psychological distress, the women will receive basic psychoeducation as well as instruction in self-care and stress management. It is expected that a significant number will improve from this intervention alone. Women who are not improving or who are initially diagnosed as suffering severe depression, suicidal ideation or other mental illness will move immediately to step two: specialized services, including individual or group counseling and/or drug therapy delivered by PCAF professionals, also at the village level. It is expected that approximately 5 percent of patients will require step three care: specialized psychological and pharmacological management by a PCAF psychiatrist at the district hospital.
Millenium Development Goals:


Questions for Discussion
1. How do you think sensitizing communities to perinatal depression will increase treatment?
2. Why do think it is important to include mental health screening in routine care?
3. How do you think this project will impact future generations in Uganda?
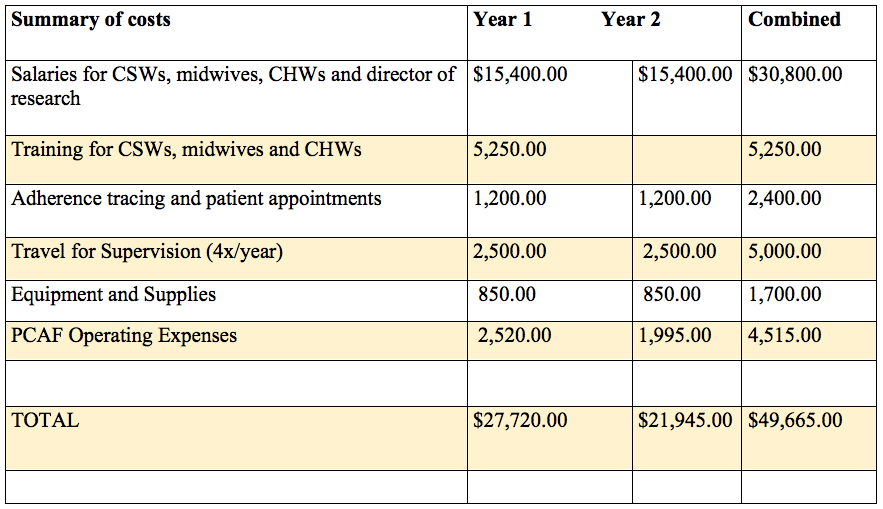
How the Grant Will be Used
DFW funding will support:
• Salaries for the Director of Research, four community outreach social workers, four midwives and 22 community health workers
• Training expenses
• Adherence tracing: The community health workers and community social workers will be using cell phones to the extent possible (a certain number of patients do not have access to cell phones) to follow-up with patients and to communicate with each other, the project manager and the clinic staff.
• Program supervision: Quarterly supervision visits costs include travel from Kampala to each clinic as well as lodging for the Director of Research.
• Equipment and supplies: Cell phones will be purchased for the CSWs and paper for data collection.
Why We Love This Project/Organization
PCAF focuses on an important issue of mental trauma among post-conflict pregnant women. Their holistic approach that focuses on building capacity in the community is well conceived, persuasive and has the potential for sustainability over time.
Evidence of Success
To date, more than 100,000 survivors of terrorism and mass violence have been treated by PCAF-trained personnel or in PCAF clinics. Patient outcome data from PCAF’s Ugandan sites since 2011 consistently demonstrates that the majority of individuals who received mental health services (including individual and group psychosocial as well as pharmacological interventions) had a sustained decline in levels of depression and PTSD symptoms and an increase in social functioning, self-care and return to work or school. This observation is even stronger for patients with multiple diagnoses. PCAF’s patient outcomes have been published in a number of academic journal articles, including PLOS Medicine, in Implementation and Scale-Up of Psycho-Trauma Centers in a Post-Conflict Area: A Case Study of a Private–Public Partnership in Northern Uganda.
Voices of the Girls
T.R. said that before PCAF she felt crippled and could not do anything. She had thoughts of committing suicide and killing her son. However, with the support from PCAF interventions, she is able to take care of herself and the son participates in domestic work. Hence she believes that it is God doing work through PCAF, without whom people like her would be doomed.
Alara
Alara had been happily married for six years when she was abducted by the Lord’s Resistance Army while fetching water. While in captivity, she was tortured and forced to beat an older woman with a stick. She witnessed killings and was made to collect the remains of those hacked to death in front of her. When she eventually returned home, her husband divorced her fearing she would kill him. Alara was admitted at PCAF’s Kitgum Clinic and was diagnosed with PTSD. Following narrative exposure therapy, antidepressants, psychoeducation and spiritual healing, her well-being improved. In her words, “I am more than my past.”
T.Z.
T.Z. is a 35-year-old female from Congo living in the Odobu refugee settlement. In 2004, rebels had attacked her village and abducted her husband, who had been working as a school teacher. She was also gang raped by five men on that day. T.Z. fled with her children to settlement camps in Uganda.
After some time, she decided to marry a fellow Congolese refugee with whom she had had a child, but soon faced domestic violence, verbal abuse, lack of financial support and mistreatment towards her children. Because of these problems, T.Z. decided to live alone as a single parent.
The patient was referred to PCAF clinic by community mobilizers. She reported feeling overwhelmed with responsibilities, not knowing where her husband is, poor relationships with her neighbors, lower abdominal pain from the gang rape, resorting to alcohol to sleep and having nightmares. Interventions included working one-on-one to assess her problems and prioritize them, including behavioral therapy, sleep hygiene, education and discussion on the adverse effects of alcohol in her life, skills training and regular home visits to asses T.Z.’s level of social functioning and alcohol consumption. Presently, the client has stopped drinking alcohol completely and has shown improved social functioning through participating in fieldwork. She also has actively enrolled in group therapy and is acting as a community mobilizer and translator to the group.
A.G.
A.G. is a 26-year old woman from Obiya village in Kitgum. She had lost her father to LRA rebels in 2002 and was abducted by the LRA in 2003. She returned home after one year in captivity and faced domestic violence from her husband, who had infected her with HIV/AIDs. After separating from her husband, A.G. was stigmatized by her community and even by her own mother for “failing” at her marriage. She took care of eight children, two of her own and six of her parents’, who struggled with alcohol abuse.
Community health workers referred A.G. to PCAF for continual sadness, poor sleep, nightmares and worries. She reported hopelessness, a sense of unworthiness, continual sadness, loss of energy and suicidal thoughts. She was diagnosed with PTSD and depression and treated with anti-depressants and outreach visits. Outreach visits were conducted to strengthen her social support from her mother and uncles. By the last session, A.G.’s family had reduced their alcohol consumption. A.G. went to work selling vegetables in the market to improve her life and that of her siblings. A.G. had become a source of encouragement to others.
Ajash
Ajash is a 24-year old Acholi woman from the Mucwini sub-county in Kitgum. She was referred to the PCAF clinic because of nightmares, headaches, constant crying, chronic chest pain and poor sleep. She was suicidal and suffered from seizures and memory impairment. Although she had not been abducted, Ajash reported living in an IDP camp in pathetic conditions where she suffered deprivation, witnessed many tortures and killings and lost a brother to violence. Ajash later married an alcoholic husband who subjected her children to child abuse. After coming to the clinic, PCAF staff diagnosed Ajash with PTSD, and began treating her with group therapy, as well as antidepressants and anticonvulsant medication. After receiving this support, Ajash no longer feels suicidal, adheres to her treatment, and has resolved to forgive, obtain new social support and find a safe space for herself and her children where she can be happy.
About the Organization
PCAF was founded in 2003 to honor the life of Peter Alderman, who was 25 when he was killed in the attacks on the World Trade Center. Peter’s family wanted to help those who had survived terrorism but had no access to care. The organization has evolved from an initial effort to train doctors from post-conflict countries to treat trauma and depression to an international NGO that builds mental health capacity in post-conflict countries and runs clinics and community-based outreaches treating tens of thousands of patients each year. President Barack Obama recognized Dr. Stephen and Elizabeth Alderman for their work with PCAF by presenting them with the Presidential Citizen’s Medal in October 2011. The Aldermans also received the 2009 Purpose Prize from Civic Ventures. In 2007, Barron’s Magazine named the Peter C. Alderman Foundation as one of the ten most effective small charities in America for its sustained measurable impact on people’s lives. PCAF has been described by one partner as “the catalyst” for bringing mental health to the forefront of the agenda for the developing world.
 PCAF works on the ground to strengthen mental health systems and advocate for improving services in developing countries where there are severely limited resources for mental health. PCAF’s approach is to establish clinics and outreaches in public-private partnership with government; train locally available caregivers to deliver evidence-based interventions in the local context; supervise and provide continuing education to staff; integrate a rigorous measurement and evaluation system; and prioritize mental health services through public awareness and annual conferences to establish a network of global mental health professionals able to advise policymakers.
PCAF works on the ground to strengthen mental health systems and advocate for improving services in developing countries where there are severely limited resources for mental health. PCAF’s approach is to establish clinics and outreaches in public-private partnership with government; train locally available caregivers to deliver evidence-based interventions in the local context; supervise and provide continuing education to staff; integrate a rigorous measurement and evaluation system; and prioritize mental health services through public awareness and annual conferences to establish a network of global mental health professionals able to advise policymakers.
In addition to PCAF’s clinic-based work, its robust community outreach program in northern Uganda includes regular twice-monthly outreaches at eleven sites at low-level government community health centers; regular social worker community visits; specialized group therapy for women and girls, former child soldiers, the elderly and people living with HIV/AIDS; and uses community mobilizers and community health workers to help with psychoeducation, screening and referrals. The mobilizers also help PCAF social workers with patient follow-up.
The PCAF Uganda clinics and their outreaches serve those most in need, who have least access to mental health care. The staff treated nearly 7,000 patients in the first three quarters of 2014. More than 70 percent of PCAF patients are women and children. The main vulnerabilities include living in an internally displaced persons’ (IDP) camp or former displacement, losing a family member to violence and experiencing physical trauma. The majority of patients have symptoms of depression (68 percent) and/or posttraumatic stress disorder (54 percent). More than 41 percent of patients were formerly abducted. Women are significantly more likely to report experiences of domestic violence and sexual and other forms of gender-based violence, while men are more likely to have been abducted and forced to torture or kill as war combatants.
Where They Work
 About the size of Oregon, Uganda is a landlocked, mountain-lined fertile plateau in Central Eastern Africa with many lakes and rivers. It is bordered by the Democratic Republic of the Congo, Kenya, Rwanda, South Sudan and Tanzania.
About the size of Oregon, Uganda is a landlocked, mountain-lined fertile plateau in Central Eastern Africa with many lakes and rivers. It is bordered by the Democratic Republic of the Congo, Kenya, Rwanda, South Sudan and Tanzania.
Overall Uganda’s climate is tropical, generally rainy with two dry seasons (December – February, June – August); although it is semiarid in the northeast. With nearly three-quarters of the land farmed, products are mostly agricultural, including coffee, tea, cotton, tobacco, cassava, potatoes, corn, millet, cut flowers, beef, goat meat, milk and poultry. Uganda’s natural resources include copper, cobalt, and hydropower, limestone, salt and gold.
Britain’s colonial boundaries grouped together a wide range of ethnic groups with different political systems and cultures. These differences prevented the establishment of a working political community after independence was achieved in 1962. The dictatorial regime of Idi Amin (1971-79) was responsible for the deaths of some 300,000 opponents. Guerrilla war and human rights abuses under Milton Obote (1980-85) claimed at least another 100,000 lives. The rule of Yoweri Museveni since 1986 has brought relative stability and economic growth to Uganda. A constitutional referendum in 2005 cancelled a 19-year ban on multi-party politics and lifted term limits.
The 35 million Ugandans are divided among a dozen major ethnic groups. In addition to genocide, their numbers have been depleted by AIDS. Most Ugandans are Roman Catholic or Protestant (42 percent each) or Muslim (12.1 percent).
English is the official national language and is taught in grade schools, used in courts of law and preferred by most newspapers and some radio broadcasts.
Source Materials
Sources: Peter C. Alderman Foundation, The CIA World Factbook.