
Mission
The mission of Village Health Partnership is to prevent maternal and neonatal death in childbirth and to treat and prevent gynecologic complications of childbirth in rural Ethiopia.
Life Challenges of the Women Served
 Ethiopia is one of the poorest countries in the world, with one of the highest rates of maternal morbidity and mortality. Village Health Partnership (VHP) targets women living in rural western and southwestern Ethiopia, some of the poorest and most remote parts of the country. In these rural areas, women work the land as illiterate subsistence farmers who live in isolated villages where they have little or no access to healthcare. From an early age, they work in the fields and carry heavy loads of wood and water on a daily basis.
Ethiopia is one of the poorest countries in the world, with one of the highest rates of maternal morbidity and mortality. Village Health Partnership (VHP) targets women living in rural western and southwestern Ethiopia, some of the poorest and most remote parts of the country. In these rural areas, women work the land as illiterate subsistence farmers who live in isolated villages where they have little or no access to healthcare. From an early age, they work in the fields and carry heavy loads of wood and water on a daily basis.
The West Omo Zone (WOZ), where VHP focuses its efforts, is one of most isolated and remote parts of Ethiopia. WOZ is home to 700,000 people, half of whom are women. WOZ consists of multiple competing pastoral and semi-pastoral tribal groups. There is little in the way of leadership or developed infrastructure.
Women in the area marry young, and without birth control, they give birth again and again. Many women give birth alone at home, and one in 10 women die in childbirth. If health facilities exist at all in this area, they are often deadly places to deliver. There is little in the way of access to water, open defecation is common, hand washing is nonexistent, surgical instruments are not sterilized, labor and delivery is not clean, and biohazard is disposed of in unfenced pits. In addition, women are often forced to sleep outside under trees in the rain waiting for delivery. Equipment and supplies are limited, and medical providers lack the skills necessary to facilitate delivery and effectively resuscitate infants.
When a woman dies in childbirth, everyone mourns the loss of a mother, a wife, a vital care provider, and an important contributor to the economic viability of the family. For people living a subsistence existence, the impact is felt by the whole community that relies on each other for survival. Those women who survive childbirth are often left with serious gynecologic injuries, including fistula. In this condition, husbands routinely divorce their wives, leaving them destitute. The shame and depth of the physical, emotional, and economic suffering are enormous.
The Project
In an effort to address the maternal healthcare needs of these women in rural Ethiopia, Village Health Partnership has three primary areas of focus:
 Screen, Transport, and Treat (STT) Program: Through this program, VHP works with members of the Western Wollega Bethel Synod Development and Social Service Committee (WWBS DASSC), medical providers, and local stakeholders to identify women with severe gynecologic complications of childbirth (specifically obstetric fistula and severe pelvic organ prolapse). Identified women are then transported to Aira Hospital where they undergo surgical treatment.
Screen, Transport, and Treat (STT) Program: Through this program, VHP works with members of the Western Wollega Bethel Synod Development and Social Service Committee (WWBS DASSC), medical providers, and local stakeholders to identify women with severe gynecologic complications of childbirth (specifically obstetric fistula and severe pelvic organ prolapse). Identified women are then transported to Aira Hospital where they undergo surgical treatment.
Water, Sanitation, & Hygiene and Maternal Health Initiative (WASH and MHI): This program involves a multi-phase effort to create year-round access to clean water, improve measures for sanitation and hygiene, and implement basic infrastructure for maternal health in 14 rural health facilities. These facilities, which form a health system of care that covers the entire WOZ in Ethiopia, include three district hospitals and 11 health centers that come under the referral umbrella of the Mizan Tepi University Teaching Hospital (MTUTH) in Mizan-Aman.
Education and Training Programs: In tandem with the WASH and MHI, VHP supports three education and training programs for rural healthcare providers. First, VHP has a scholarship program for village women who wish to become nurse-midwives and serve in the rural areas. Second, nurse-midwives practicing on the front lines are offered three weeks of intensive skill building using the Jhpeigo* Basic Emergency Maternal Obstetric and Neonatal Care (BEMONC) curriculum. Finally, VHP is implementing a Skill Check, Training, and Mentorship Program. All of VHP’s education and training programs aim to create a competent work force that can provide skilled assistance at the time of delivery. (*Originally known as the Johns Hopkins Program for International Education in Gynecology and Obstetrics, Jhpeigo is a leader in reproductive health training.)

Together Women Rise’s grant will support the Skill Check, Training, and Mentorship Program and BEMONC Training. Through these two programs, VHP aims to give pregnant women access to skilled assistance at the time of delivery and ultimately reduce rates of maternal and neonatal morbidity and mortality in this remote area of Ethiopia. The program will target two nurse-midwives in each of eight healthcare facilities in the WOZ four times per year with obstetric and neonatal skill checks and on-the-spot training.
Skill Check: Experienced nurse-midwife trainers from MTUTH visit rural health clinics to perform skill checks on nurse-midwives. Using elements of Jhpiego’s BEMONC Training Program curriculum, trainers test two nurse-midwives in each of eight rural health facilities on specific core obstetric and neonatal skills, including active management of the third stage of labor, breech delivery, pre-eclampsia and eclampsia, bag and mask skill check, and more. Test scores for the skill checks are recorded and tracked.
The nurse-midwife trainers provide on-the-spot training to local nurse-midwives when they visit rural healthcare facilities. This training is focused in response to the skill checks of the targeted nurse-midwives.
Mentorship: The nurse-midwives in each facility are actively linked to mentors at MTUTH, who are available for questions and to support them with difficult cases. The nurse-midwives who have been tested and trained then support, teach, and mentor their colleagues.
BEMONC Training: Nurse-midwives who need more intervention will be referred to VPH’s BEMONC Training at MTUTH. This training provides a three-week, hands-on, intensive training for 20 nurse-midwives each year.
Year 1 – Direct Impact: 84 (nurse-midwives); Indirect Impact: 350,000 (community members)
Year 2 – Direct Impact: 84 (nurse-midwives); Indirect Impact: 350,000 (community members)
UN Sustainable Development Goals
![]()
![]()
![]()
![]()
![]()
![]()
Questions for Discussion
 How do you think training nurse-midwives in rural communities will impact the community, both in terms of maternal healthcare and other ways?
How do you think training nurse-midwives in rural communities will impact the community, both in terms of maternal healthcare and other ways?- Why do you think it is important that the nurse-midwives have connections to the community in which they work?
- Why do think a village woman would pursue a career as a nurse-midwife, especially knowing the challenges they face?
How the Grant Will be Used
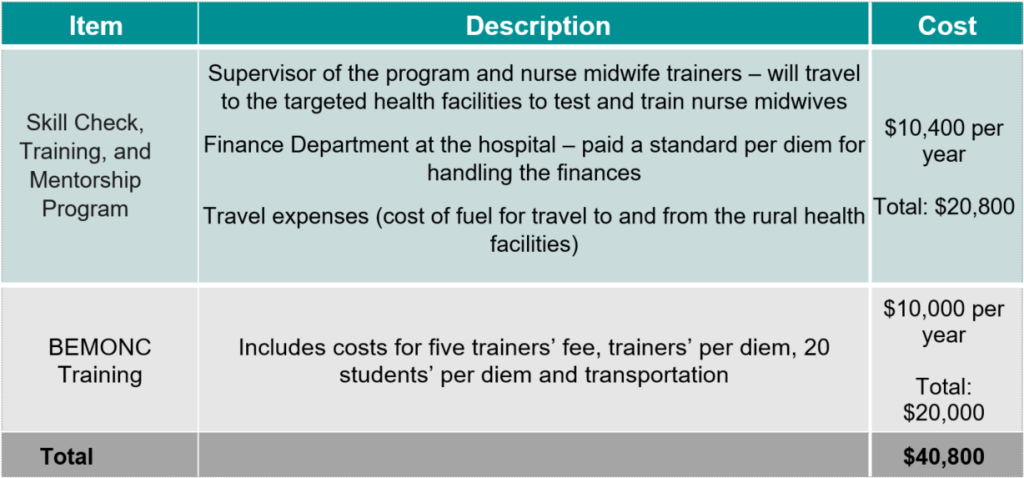
Together Women Rise’s grant of $40,800 for two years will fund the following:
Why We Love This Project/Organization
We love this project’s focus on interventions to prevent maternal morbidity and mortality. Village Health Partnership works to strengthen health care services, build capacity, and improve WASH (Water, Sanitation, and Hygiene), healthcare provider training, and patient care. VHP also works on the barriers to care, such as the decisions to access care, transportation to medical facilities, and the availability of timely care.
Evidence of Success
Since 2010, Village Health Partnership has:
- Implemented a scholarship program for village women who wish to become nurse-midwives. To date VHP has supported 22 women with three-year scholarships and five women with a year of tutoring so that they can pass their certification exam.
- Implemented skill building programs for nurse-midwives on the front lines. VHP has held three-day training sessions using the American Academy of Pediatrics Helping Babies Breathe (HBB) and three-week training sessions using the Jhpiego BEMONC curriculum. To date VHP has trained 11 Master Trainers, more than 250 nurse-midwives in HBB, and more than 180 nurse-midwives in the BEMONC curriculum.
- Screened, transported, and treated more than 800 women with severe gynecological complications of childbirth, including obstetric fistula. The STT Program is now considered to be a “flagship” program for all of Ethiopia.
- Constructed a gynecology ward and operating room at Aira Hospital and supported the facility to become a center of excellence for women’s health in the western part of the country.

- Constructed a maternity waiting area and purchased a generator for the MTUTH. VHP has conducted research on maternal healthcare and published multiple papers in peer reviewed journals that reveal that the hospital is doing a good job with few resources. VHP supported the facility to become a center of excellence for women’s health in the southwest part of the country.
- Implemented infrastructure for WASH and maternal health in nine health facilities including three district hospitals and six health centers. As a result, a health system of care is now emerging in the WOZ. The effort is giving pregnant women access to clean and safe healthcare and skilled assistance at the time of delivery, including access to emergency obstetric care.
Voices of the Girls
From VHP: “Stories like Asha Ahimad are common to the women we serve. Mrs. Asha was married at a very early age. Her first delivery resulted in a stillbirth and severe gynecologic complications. At the time of delivery, she was taken to a nearby health center that was unable to care for her. She was then referred to the nearest district hospital, but by that point her situation was too far along. They were able to save her life by performing a caesarian section but were unable to save her baby. She developed fistula due to the prolonged delivery, was incontinent, and had to use a urine drainage bag. She endured severe emotional suffering and isolated herself from her community. Mrs. Asha was identified through our STT Program and received treatment in 2021. She is now happily reintegrated with her family and village.”
About the Organization
VHP was founded in 2010 when community leaders in Ethiopia approached the founder and president, Margaret “Migs” Muldrow, MD, to partner with them to improve maternal health. Having grown up in the country, Dr. Muldrow has a deep knowledge of Ethiopia’s culture, language, and medical needs. She has remained connected to Ethiopia as an adult. Dr. Muldrow knew she was in a unique position to help tackle the challenges faced by women living in some of the poorest and most remote parts of Ethiopia.
A group of doctors and area experts came together in 2010 to form a board and launch VHP. The initial program offered was a Screen, Transport, and Treat (STT) Program, which continues today and provides direct healthcare services to women suffering from gynecologic complications of childbirth. VHP first provided services to only a few women at a time, but the program has grown to now serve 175+ women throughout rural western Ethiopia each year.

Through this fieldwork, it became clear that prevention efforts were key to reducing maternal morbidity and mortality. Access to clean, safe, and competent healthcare at the time of delivery was critical. Unfortunately, after deep needs assessments, VHP was confronted with the marginal capacity of the healthcare system in rural western Ethiopia, including unsafe conditions in existing health facilities – no access to water and complete lack of measures for sanitation and hygiene; no infrastructure for maternal health, minimal equipment on labor and delivery, and no place for women to stay while they labored; and a lack of skilled healthcare providers. The few nurse-midwives that existed lacked the ability to provide competent assistance with delivery and care of neonates.
In response, VHP launched a Water, Sanitation, and Hygiene & Maternal Health Initiative (WASH & MHI) in 2017 in the West Omo Zone (WOZ) of southwestern Ethiopia. Working with community stakeholders, they are now implementing year-round access to water, measures for sanitation and hygiene, and infrastructure for maternal health in 14 health facilities. As part of the initiative, VHP has incorporated a skill-building education and training curriculum that targets nurse-midwives on the front lines. The three district hospitals and 11 health centers where VHP works form a health system of care that covers the entire WOZ. The effort gives pregnant women access to life-saving skilled assistance at the time of delivery and emergency obstetric care. The initiative ultimately impacts all 700,000 residents of the WOZ.
Where They Work

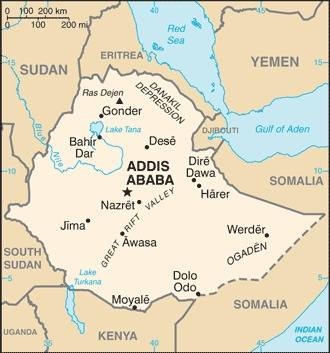
The 2023 estimated population of Ethiopia is more than 116 million people. Ethiopia is a predominantly agricultural country – nearly 80 percent of the population lives in rural areas – that is in the early stages of demographic transition. Infant, child, and maternal mortality have fallen sharply over the past decade, but the total fertility rate has declined more slowly, and the population continues to grow. While the use of modern contraceptive methods among married women has increased significantly from 6 percent in 2000 to 27 percent in 2012, the overall rate is still quite low. Ethiopia’s rapid population growth is putting increasing pressure on land resources, expanding environmental degradation, and raising vulnerability to food shortages. About 40 percent of the population is below the age of 15 and the country has a fertility rate of four children per woman (and even higher in rural areas).
Ethiopia has a growing economy, but is still one of the poorest countries in the world, with a per capita annual income of $960. According to the World Bank, about 24 percent of Ethiopians were living below the national poverty line in 2016, but inequality has increased in recent years, and about half of the adult population of Ethiopia is facing severe food insecurity. There are ongoing conflicts in multiple parts of the country, making access to services such as safe and effective healthcare extremely challenging.
- Birthrate: 29.97 births/1,000 population (2023 est.)
- Mother’s mean age at first birth: 19.3 years (2019 est.)
- Maternal mortality ratio: 401 deaths/100,000 live births
- Infant mortality ratio: 32.44 deaths/1,000 live births
- Literacy rate: total population 51.8 percent, male: 57.2 percent, female 44.4 percent.
A closer look at barriers to maternal care
Although the United Nation’s Millennium Development Goals aimed to reduce global maternal mortality ratios by 75 percent by 2015, there are still 830 women dying every day worldwide from preventable causes due to improper maternal care. In 2010, 287,000 women died during and following pregnancy and childbirth. Almost all maternal deaths (99 percent) occur in developing countries. More than half of these deaths occur in Sub-Saharan Africa where maternal mortality is still a persisting challenge.
Poor women in remote areas are the least likely to receive adequate health care. This is especially true for regions with low numbers of skilled health workers. While levels of antenatal care have increased in many parts of the world during the past decade, only 46 percent of women in low-income countries have the benefit of skilled care during childbirth. This means that millions of births are not assisted by a midwife, a doctor, or a trained nurse.
Research shows that the most important barriers to maternal health are transportation to health facilities, economic factors, and cultural beliefs. Other factors that prevent women from receiving or seeking care during pregnancy and childbirth are lack of information and inadequate services. The World Health Organization reports that the most important interventions in this maternal mortality are birth control, access to skilled assistance at the time of delivery, and access to emergency obstetric care.
To improve maternal health, barriers that limit access to quality maternal health services must be identified and addressed at all levels of the health system.
Source Materials

