
Mission
Brick by Brick Partners creates partnerships that improve education, health, and economic opportunity in East Africa.
Life Challenges of the Women Served
Every year 6,000 women die in Uganda due to entirely treatable complications of pregnancy and childbirth. That’s 16 women every day who are leaving orphaned children behind – with a fertility rate of 6.9 children per woman, that’s a lot of children who will grow up motherless. This is compounded by the fact that 45,000 infants every year have a high risk of dying at less than a month old from infections, birth asphyxia and injuries, and complications of prematurity. The risk of a mother dying in Uganda is 14 times greater than the risk in the U.S. and 50 times greater than in Canada. Three out of four of these deaths can be attributed to the delay in deciding to seek skilled maternity and newborn care, accessing this care once the decision is made, or receiving quality care once a health facility is reached.
 The first two of these delays are often related to transportation. Uganda’s Rakai and Kyotera Districts are entirely rural, with extremely under-developed roads and transportation infrastructure. Over 90 percent of residents in these areas live in remote villages, often many miles from a health facility staffed by a skilled birth attendant. With the exception of one paved road that connects Rakai to Masaka, all others are poor dirt roads. For many communities, there are no roads at all. This region of Uganda has two rainy seasons, each lasting 2 – 3 months. During these periods of heavy storms, these already poor roads may become slippery, wash away, or become impassable. In these districts there are only two ambulances for over half a million people, and they often lack gasoline. All of these factors increase the delays of laboring mothers in reaching health facilities.
The first two of these delays are often related to transportation. Uganda’s Rakai and Kyotera Districts are entirely rural, with extremely under-developed roads and transportation infrastructure. Over 90 percent of residents in these areas live in remote villages, often many miles from a health facility staffed by a skilled birth attendant. With the exception of one paved road that connects Rakai to Masaka, all others are poor dirt roads. For many communities, there are no roads at all. This region of Uganda has two rainy seasons, each lasting 2 – 3 months. During these periods of heavy storms, these already poor roads may become slippery, wash away, or become impassable. In these districts there are only two ambulances for over half a million people, and they often lack gasoline. All of these factors increase the delays of laboring mothers in reaching health facilities.
Twenty-nine percent of Rakai and Masaka residents live more than three miles (5 km) from a public health facility, which in itself poses a serious access issue. In addition, 14 percent of births are considered high risk because they occur too close to each other and arise from low contraceptive use. Poverty and a lack of education also contribute to negative outcomes. One out of four Rakai and Kyotera residents live in extreme poverty, often due to reduced productivity from agriculture, the major economic activity. Over 80 percent are engaged in subsistence farming. A third of women 18 and older are illiterate. These poor rural women are more likely to marry young, less likely to attend antenatal care or deliver in health facilities, and less likely to be able to afford transportation to a health center or hospital when emergencies occur. The consequences of delays are dire, as by the time these patients reach healthcare facilities, many have already sustained life-threatening injuries, often leading to the death of mother and baby or life-long disability such as obstetric fistulae or cerebral palsy.
 The lack of access to adequate transportation for these women is of grave concern to the district and national government and various members of the community. However, current public and Ugandan government resources are inadequate to address this health crisis. As a result, a number of women describe their experiences as very traumatic and life threatening. There are 25,000 deliveries in Rakai and Kyotera every year. Half, or 12,562, of these laboring women require transportation to health centers, and approximately 1,900 (15 percent) require emergency transport to a higher-level facility. Adolescents are especially at risk for obstetric complications and a lack of access to affordable transportation. Currently Rakai and Kyotera have a teenage pregnancy rate of 13 percent, with 15.5 percent of girls ages 12-19 having already given birth.
The lack of access to adequate transportation for these women is of grave concern to the district and national government and various members of the community. However, current public and Ugandan government resources are inadequate to address this health crisis. As a result, a number of women describe their experiences as very traumatic and life threatening. There are 25,000 deliveries in Rakai and Kyotera every year. Half, or 12,562, of these laboring women require transportation to health centers, and approximately 1,900 (15 percent) require emergency transport to a higher-level facility. Adolescents are especially at risk for obstetric complications and a lack of access to affordable transportation. Currently Rakai and Kyotera have a teenage pregnancy rate of 13 percent, with 15.5 percent of girls ages 12-19 having already given birth.
The Project
 Brick by Brick’s (BBB) Mama Rescue Project aims to reduce the delays laboring women in Rakai and Kyotera encounter in reaching a health facility, as well as the delays women encounter when they are referred from a health facility to a hospital. By addressing these delays, BBB expects to reduce obstetric complications and dramatically reduce maternal and newborn morbidity and mortality. This program was successfully piloted in other areas of Uganda between 2015 and 2017, resulting in an increase in prenatal care and a 33 percent decrease in stillbirths in the first year alone.
Brick by Brick’s (BBB) Mama Rescue Project aims to reduce the delays laboring women in Rakai and Kyotera encounter in reaching a health facility, as well as the delays women encounter when they are referred from a health facility to a hospital. By addressing these delays, BBB expects to reduce obstetric complications and dramatically reduce maternal and newborn morbidity and mortality. This program was successfully piloted in other areas of Uganda between 2015 and 2017, resulting in an increase in prenatal care and a 33 percent decrease in stillbirths in the first year alone.
The Mama Rescue Project (MRP) is the natural outgrowth of Brick by Brick’s highly successful Babies and Mothers Alive (BAMA) program that has already dramatically reduced maternal and newborn mortality and morbidity in the Rakai and Kyotera Districts. Maternal mortality alone has been reduced by 60 percent. Since 2015, this program has partnered with the Ugandan Ministry of Health and health providers at the 48 health centers and hospitals in the districts. Major program interventions include health provider clinical skills trainings and mentorships, distribution of life-saving medical supplies and equipment, and maternal and newborn health performance reviews. BAMA also implements community mobilizations through their highly trained Mama and Papa Ambassadors, Village Health Teams, radio talk shows to create and increase demand for institutional health services, and support of local health facility ambulances for transport to health facilities for women and/or newborns suffering complications of pregnancy and childbirth.
The issue now is how – or how fast – women can access this life-saving care for themselves and/or their newborns. To meet the needs of these women, Brick by Brick will initiate three key elements that, together, define the Mama Rescue Project:
 Facility-Based Delivery: Mama Rescue will provide transport vouchers to women enrolled in the system after attending their fourth prenatal visit. These vouchers guarantee free transport by boda boda (motorcycle taxi) from home to a health center for delivery with a skilled midwife. BAMA has documented that mothers who attend four prenatal visits are 81 percent more likely to deliver in one of BBB’s partnering health facilities. Patient transport utilizing motorcycle and automobile taxis has been proven safe and culturally acceptable in other similar settings.
Facility-Based Delivery: Mama Rescue will provide transport vouchers to women enrolled in the system after attending their fourth prenatal visit. These vouchers guarantee free transport by boda boda (motorcycle taxi) from home to a health center for delivery with a skilled midwife. BAMA has documented that mothers who attend four prenatal visits are 81 percent more likely to deliver in one of BBB’s partnering health facilities. Patient transport utilizing motorcycle and automobile taxis has been proven safe and culturally acceptable in other similar settings.- Rapid Emergency Response: Midwives at 22 Health Center IIIs and three District Hospitals will use their mobile phones to request emergency transport, using an automatic dispatch USSD-based system (Unstructured Supplementary Service Data). Local taxi drivers will be alerted by mobile phone text. A driver with boda boda is selected based on the quickest response time. Upon transporting the woman to the receiving facility, the midwife will verify the driver immediately and initiate payment with mobile money for the transport service rendered. Automobile taxis will be enrolled as well to serve as ‘ambulances’ when emergency referral from health center to hospital is required and a proper ambulance is not available.
- Communication of Critical Information: Referring midwives will use the Mama Rescue menus on their phones to send summary clinical information to the hospital, ahead of the woman’s arrival. This enables the hospital midwives and physicians to prepare for the admission and reduce the wait time for services such as surgical procedures and blood transfusions.
 Since Mama Rescue uses simple USSD-based technology and locally available infrastructure (simple phones, local transport, and mobile money), this program is readily adaptable and scalable to other regions, countries, communities, and public health issues. Although the internet is widely available all over the country, there are areas with no service and a majority of the rural population lacks access. This further justifies use of the USSD-based system. In fact, only six percent of women in Rakai use the internet, while access to cellphones is at 65 percent for men and 47 percent for women. The level of mobile phone access keeps increasing and today almost every woman has access to a phone through a relative or community member. The Mama Rescue Project also involves several key partners, including the Rakai and Kyotera Districts health departments, the Uganda Ministry of Health, MTN, Yo Uganda, existing taxi driver associations, as well as numerous Village Savings and Loan Associations (VSLA) throughout participating communities. The program leverages local resources, such as existing boda boda and taxi systems, VSLAs, and a previously well-trained cadre of health providers and Mama Ambassadors.
Since Mama Rescue uses simple USSD-based technology and locally available infrastructure (simple phones, local transport, and mobile money), this program is readily adaptable and scalable to other regions, countries, communities, and public health issues. Although the internet is widely available all over the country, there are areas with no service and a majority of the rural population lacks access. This further justifies use of the USSD-based system. In fact, only six percent of women in Rakai use the internet, while access to cellphones is at 65 percent for men and 47 percent for women. The level of mobile phone access keeps increasing and today almost every woman has access to a phone through a relative or community member. The Mama Rescue Project also involves several key partners, including the Rakai and Kyotera Districts health departments, the Uganda Ministry of Health, MTN, Yo Uganda, existing taxi driver associations, as well as numerous Village Savings and Loan Associations (VSLA) throughout participating communities. The program leverages local resources, such as existing boda boda and taxi systems, VSLAs, and a previously well-trained cadre of health providers and Mama Ambassadors.
The Mama Rescue Project allows Brick by Brick to launch a pilot project to provide transportation from village to health center for 6,281 pregnant and laboring women. The anticipated benefits are far-reaching and life-saving:
 80 percent of the 6,281women in need of transportation from home to health center will be served
80 percent of the 6,281women in need of transportation from home to health center will be served- 100 percent of women in need emergency referral will be served
- A functional transportation and referral system in the two districts of Rakai and Kyotera
- One-hour transit time from home to health center
- Less than one-hour transit time from health center to hospital for emergency situations
- 30 percent reduction in pregnancy-related hemorrhage
- 30 percent increase in antenatal and postnatal care attendance
- 25 percent increase in attendance at all four antenatal care visits above current levels
- Improved emergency response at Brick by Brick’s 25 participating health facilities
- Improved emergency preparedness level in all health facilities
- More institutional (professionally assisted) deliveries.
All pregnant women attending prenatal clinics at BBB’s 25 participating health facilities will be provided with information regarding participating in the Mama Rescue Project. They will be offered an application/survey questionnaire to complete. This will assess their distance from home to the nearest participating health center and their economic status, which will determine eligibility for Mama Rescue. Poor women, who are expected to comprise half the pregnancies, will be eligible for a delivery voucher. Upon attendance at the fourth prenatal visit, those women previously deemed eligible will be given an individual voucher number and oral and written/pictorial instructions on how to use the Mama Rescue platform. Any woman experiencing a complication at any participating health center, either before, during or after labor, will be provided with a transport voucher number, and the referring health provider will call the nearest Mama Rescue automobile taxi or ambulance if available.
The Mama Rescue Project is a proven innovation that affordably addresses the need for emergency transportation for women in labor and those patients requiring emergency referral from rural health centers to hospitals. At the heart of this program is full partnership with local government and the civil society. BBB will fully engage and strengthen existing VSLAs who they believe are capable of generating the savings that can cover the cost of transport for women in need ($3 USD). BBB anticipates that the cost of emergency transport will require a cost sharing model involving district government, corporate sponsors, foundation support and on-going funding by Brick by Brick Partners.
Direct Impact: 6,281 women in labor, Indirect Impact: 50,543 (midwives, Mama Ambassadors, motorbike drivers, spouses, and children)
UN Sustainable Development Goals
![]()
![]()
![]()
![]()
![]()
Questions for Discussion
- What benefits might occur beyond improving maternal and newborn outcomes?
- Why are partnerships pivotal to the success of this program?
- What other issues might be addressed using the technology in the Mama Rescue Project?
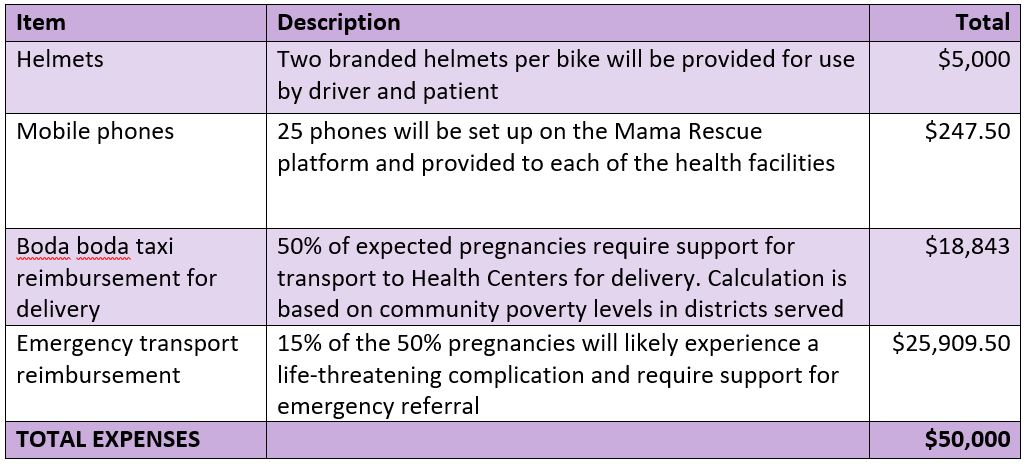
How the Grant Will be Used
The total budget project budget and DFW’s grant is $50,000 for one year.
Why We Love This Project/Organization
We love this project because it reduces the time for laboring women to access emergency obstetric care. The Mama Rescue Project will lead to better health outcomes for mothers and babies. We love that Brick by Brick Partners builds this important infrastructure in these communities by incentivizing the utilization of health care and by employing innovative referral systems and mobile technology.
Evidence of Success
 Over its 15 years of work in the rural communities of Rakai and Kyotera, BBB has steadily expanded the scope and impact of its programs. Since 2011, with an expanded mission to create partnerships that improve education, health and economic opportunity, BBB’s programs have increasingly focused on the health and full empowerment of women. The work is the result of fully engaged partnerships with the local government and the institutions and rural communities where the impact is most felt.
Over its 15 years of work in the rural communities of Rakai and Kyotera, BBB has steadily expanded the scope and impact of its programs. Since 2011, with an expanded mission to create partnerships that improve education, health and economic opportunity, BBB’s programs have increasingly focused on the health and full empowerment of women. The work is the result of fully engaged partnerships with the local government and the institutions and rural communities where the impact is most felt.
BBB has been recognized through grant awards by the United States Department of State/PEPFAR, the Government of Canada through their Grand Challenges Canada Program, and the ELMA Foundation. Brick by Brick Uganda is registered as an NGO with the Government of Uganda, and is a member of various working groups at the Ministry of Health in which the senior staff (Executive and Clinical Directors) participate in the following areas: Maternal Child Health Cluster, Non-Communicable Diseases Technical Working Group; Adolescent Health Working Group; Family Planning Working Group; Mental Health Working Group among others. BBB is also a member of the Uganda Water and Sanitation Network, National NGO forum, and District NGO forums. On invitation, BBB’s Executive Director attends high level project steering committee meetings on Reproductive Maternal Child Health Programs run by the Ministry of Health.
Voices of the Girls
 “For my first pregnancy, I walked to the health center and by the time I got there we tried in vain, but my baby was too big. We were told to go to the hospital in Kalisizo but finding a boda rider was so hard and he took long. We had to go four people on the motorcycle and yet I could feel my baby coming. By the time we reached the hospital, they tried all they could, but we lost the baby because he had become distressed. For my second baby, I moved to the health center as soon as I felt pains, I still walked there. When I arrived, the midwife checked on me and when she realized I wouldn’t be able to deliver from there, she called the ambulance from Kalisizo hospital and they came and took us to the hospital. The midwife was with me and escorted me up to the hospital and was there until I delivered.”
“For my first pregnancy, I walked to the health center and by the time I got there we tried in vain, but my baby was too big. We were told to go to the hospital in Kalisizo but finding a boda rider was so hard and he took long. We had to go four people on the motorcycle and yet I could feel my baby coming. By the time we reached the hospital, they tried all they could, but we lost the baby because he had become distressed. For my second baby, I moved to the health center as soon as I felt pains, I still walked there. When I arrived, the midwife checked on me and when she realized I wouldn’t be able to deliver from there, she called the ambulance from Kalisizo hospital and they came and took us to the hospital. The midwife was with me and escorted me up to the hospital and was there until I delivered.”
- Nabakomeko Max, mother of a 1-year-old daughter
About the Organization
 BBB is an innovative bi-national partnership between Brick by Brick Partners, a US-based 501(c) (3) non-profit, and Brick by Brick Uganda, a community-based NGO registered with the Government of Uganda. The organization was founded by Drs. Daniel Murokora and Marc Sklar in 2003 to create partnerships to improve education, health, and economic opportunity in the Rakai and Kyotera Districts of Uganda. While working for the Rakai Health Sciences Program on cervical cancer research, Daniel and Marc observed that most government-funded schools in the area had old and crumbling infrastructure. The two physicians created partnerships between school communities in the United States and Uganda to rebuild four schools serving 2,000 children. Given the overwhelming need in comparison to the available resources, they designed a partnership model with the community through a cost-sharing approach in order to support more schools as well as ensure sustainability. Over the past 15 years, BBB broadened the scope of its work beyond its initial school program to include nine Universal Primary Education schools, completely rebuilding their physical infrastructure and improving literacy through their Library Project.
BBB is an innovative bi-national partnership between Brick by Brick Partners, a US-based 501(c) (3) non-profit, and Brick by Brick Uganda, a community-based NGO registered with the Government of Uganda. The organization was founded by Drs. Daniel Murokora and Marc Sklar in 2003 to create partnerships to improve education, health, and economic opportunity in the Rakai and Kyotera Districts of Uganda. While working for the Rakai Health Sciences Program on cervical cancer research, Daniel and Marc observed that most government-funded schools in the area had old and crumbling infrastructure. The two physicians created partnerships between school communities in the United States and Uganda to rebuild four schools serving 2,000 children. Given the overwhelming need in comparison to the available resources, they designed a partnership model with the community through a cost-sharing approach in order to support more schools as well as ensure sustainability. Over the past 15 years, BBB broadened the scope of its work beyond its initial school program to include nine Universal Primary Education schools, completely rebuilding their physical infrastructure and improving literacy through their Library Project.
BBB programs include:
- Babies and Mothers Alive (BAMA) Program: The BAMA Program is a vital partnership with the Ugandan Ministry of Health to dramatically reduce maternal and newborn mortality and morbidity in the Rakai and Kyotera Districts. BAMA addresses the three major delays impacting maternal and newborn health: delay to seek care, delay to access care, and delay to receive quality care at a health facility. These three delays directly or indirectly are the root causes of almost all maternal and newborn morbidity and mortality in the developing world.
- My Pads Program: The My Pads Program partners with the Ugandan Ministries of Health and Education to run a nine-week co-educational afterschool program focusing on sexual and reproductive health (SRH), gender equality, and the promotion of healthy life choices. This program culminates in the fabrication of a set of four reusable menstrual pads by the students. BBB has also constructed rainwater harvesting systems and gender-sensitive changing rooms in 16 schools to support menstrual hygiene, and it launched a Seamstress Project, training local seamstresses to fabricate machine-made reusable menstrual pads in eight communities.
- Schools Program: The Schools Program partners with the Ugandan Ministry of Education to select Universal Primary Education schools in the Rakai and Kyotera Districts for renovation and rebuilding. All construction is done by the Brick by Brick Construction Company, utilizing environmentally sustainable appropriate technology.
- Brick by Brick Construction Company: Established in 2011, this innovative social enterprise is proving that a commitment to the Triple Bottom Line – People, Planet and Profit – can work. Brick by Brick utilizes an environmentally sustainable technology, Interlocking Stabilized Soil Bricks, that helps fight deforestation and the eradication of wetlands. Brick by Brick’s masons have completed over 150 projects throughout Uganda, providing safe, clean water for over 100,000 people. All profits are re-invested back to Brick by Brick’s programs or distributed to their staff of 30 through their profit-sharing plan.
- In partnership with the United States Peace Corps, Brick by Brick developed and implemented the Lead Organize Integrate Library Training Workshop, to help schools fully utilize their school libraries in 14 schools throughout Uganda. BBB also installed solar power lighting systems in 10 primary and secondary schools, providing light for the first time for thousands of students.
Where They Work

Uganda is a landlocked country a little smaller than the state of Oregon but home to over 35 million people. Most live in the central and southern regions, particularly along the shores of Lake Victoria and Lake Albert. The population is young and among the fastest growing in the world, with the median age just 15 years old. Although the official language is English, there are more than 30 indigenous languages spoken.
The Ugandan landscape is mostly plateaus surrounded by mountains. It contains substantial natural resources, including arable land where 80 percent of the workforce is employed. Uganda shares borders with five countries: the Democratic Republic of the Congo, Kenya, Rwanda, Tanzania, and South Sudan. The Acholi region of northern Uganda is recovering from a 22-year-long armed conflict between the Lord’s Resistance Army rebels, led by Joseph Kony, and the government of the republic of Uganda. The instability and influx of refugees in neighboring Sudan have had a serious effect on Uganda, as Sudan was Uganda’s primary export partner.
Uganda is one of the poorest countries in the world, with 38 percent of the population living on less than $1.25 a day. Poverty is especially pronounced in the rural areas, where women not only work in the agricultural sector, but also take care of their families. The average Ugandan woman spends nine hours a day on domestic tasks, including cooking, fetching water and firewood, and caring for children, the elderly, the sick, and orphans. Some women attempt to supplement their incomes by rearing animals, but finding the time is challenging. Gender inequality is a fact of life in Uganda. Because of this, many women are unable to attain higher education, participate in community life, or break away from abusive husbands. Many Ugandans have emigrated to southern or western Africa looking for jobs, security, and an escape from poverty.
The two districts of Rakai and Kyotera have a total population 518,008 of which 264,954 are female. There are 104,294 women of reproductive age with 25,900 expected pregnancies and 25,123 births. As is the case elsewhere in Uganda, young people comprise the majority of the population: 57 percent are under age 17, 76 percent are 30 years and under, and adolescents 10 – 17 account for 22 percent. Thirteen percent of children 6 – 12 are in primary school, while only 30 percent of 13 – 18 year-olds are in secondary school.
 A closer look at childbirth in developing countries.
A closer look at childbirth in developing countries.
According to the World Health Organization (WHO), 99 percent of all maternal deaths occur in developing countries. Every day, 830 women in developing countries die from childbirth or pregnancy-related complications. That’s 35 women every hour of every day. And for every woman who dies from pregnancy or childbirth-related complications, 20 more suffer from childbirth-related illness or injury. Adolescent girls are particularly at risk for pregnancy complications and difficulties giving birth – an issue that, unfortunately, is all too common in developing countries. Sub-Saharan Africa has the highest maternal mortality rate in the world, followed by South-Asia. Nigeria and India alone account for one third of global maternal deaths.
Why do women in developing countries suffer from childbirth complications at alarmingly high rates? For one, high fertility rates are directly correlated with high maternal mortality rates. The more babies a woman has, the more likely she is to suffer from anemia, nutritional deficiency, hemorrhage, or a ruptured uterus – all life-threatening illnesses without adequate treatment. Furthermore, the majority of women who die during childbirth live in rural communities, where access to skilled medical workers or adequate reproductive health services and education is lacking or does not exist. Sadly, a woman’s chances of dying during childbirth increase further if she is illiterate and lives without access to clean drinking water and sanitation. The sad truth is that women are dying during childbirth because of the cruelty and inequality that comes with poverty.
But there is hope. Since 1990, the number of women dying from childbirth-related complications has decreased by 44 percent. Additionally, WHO is working to bring reproductive, maternal, and newborn healthcare to the women and girls who need it most. In 2015, the UN set global goals to “commit countries to reduce maternal deaths to fewer than 70 for every 100,000 live births.” The UN also called to end child marriage and ensure universal access to reproductive healthcare. This global commitment – along with nonprofit and governmental support – can help save the planet’s most vulnerable and marginalized mothers.
Source Materials
https://www.cia.gov/library/publications/the-world-factbook/geos/ug.html
http://www.jlof.net/about-jlof/about-uganda-and-acholiland/
https://www.who.int/news-room/fact-sheets/detail/maternal-mortality
https://www.unicef.org/media/media_47145.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5674830/
https://www.worldpress.org/africa/3834.cfm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5461715/
https://www.theguardian.com/global-development/2018/sep/24/why-do-women-still-die-giving-birth
