
About the Together Women Rise Grants Program
Together Women Rise’s Grants Program has two key components that support our overall mission to achieve global gender equality. Featured Grants are largely focused on delivering direct services by funding grassroots organizations that empower and support women and girls in low-income and marginalized countries in the Global South. Our Transformation Partnerships are designed to invest in areas where we can make the biggest impact on achieving global gender equality by addressing the root causes of gender inequality.
 Through our Featured Grants Program, we highlight a different organization/project each month, providing a variety of learning materials on the issue and how the grant will be used.
Through our Featured Grants Program, we highlight a different organization/project each month, providing a variety of learning materials on the issue and how the grant will be used.
Featured Grants may include:
- Project grants to fund a specific project or a particular deliverable for a specific timeframe; or
- General Operations grants to cover an organization’s day-to-day, ongoing expenses, such as salaries, utilities, office supplies, and more; or
- Capacity-building grants to strengthen an organization’s systems and thereby increase its effectiveness.
The Global Issue
Maternal and Newborn Health
Although important progress has been made in the last two decades, a maternal death* occurred almost every two minutes in 2020 – approximately 287,000 women globally during and following pregnancy/childbirth. And most maternal deaths are preventable with timely management by a skilled health professional working in a supportive environment. When maternal injuries (such as obstetric fistula) and deaths occur, the most common direct causes are excessive blood loss, infection, high blood pressure, unsafe abortion, and obstructed labor, as well as indirect causes such as anemia, malaria, and heart disease.
While neonatal deaths have decreased by 44 percent since 2000 and 53 percent since 1990, the first month of life is still the most vulnerable period for a child’s survival, with 2.3 million newborns dying in 2022, equating to nearly half of all deaths in children under age 5. That means approximately 6,300 newborns die every day, most (75 percent) in the first week of life.
| Among industrialized countries, the United States has the highest maternal mortality rate, with pregnant women from historically marginalized racial and ethnic groups suffering the highest rates of maternal mortality and morbidity.*
*A maternal death is defined as the death of a woman while pregnant or within 42 days of termination of pregnancy, from any cause related to the pregnancy but not from accidental or incidental causes. (The exact number in the United States is a matter of dispute, but experts agree that most maternal deaths – no matter the country – are preventable.) |
What saves the lives of mothers and babies? Access to skilled care. Remote locations or facilities without skilled birth attendants (SBAs) can mean women give birth without even basic support, too often resulting in death or injury.
A recent study published in The Lancet Global Health showed that at least 40 million women are likely to experience a long-term health problem caused by childbirth, including obstetric fistula. Obstetric fistula is a hole between the vagina and bladder or rectum that is caused by prolonged, obstructed labor. It leaves a [i]woman incontinent of urine, feces, or both. Largely eradicated with access to timely, managed care, obstetric fistula is still devastating the lives of women in the poorest countries. Corrective surgery is the only cure.
Globally, one million women suffer from fistula because they cannot access the surgery that can permanently cure them. An estimated 100,000 new women develop obstetric fistula each year. Since women typically develop fistula in their early 20s, timely intervention and surgical repair can allow a woman to reclaim 40 years or more of health and productivity, preventing decades of mental and physical suffering.
About Our Grantee
This month, Together Women Rise is funding two featured grantees: Fistula Foundation and One Heart Worldwide. We are proud to have a long history of supporting the work of both these organizations, dating back to the early days of Together Women Rise. We first funded Fistula Foundation in 2004 and subsequently awarded a Featured Grant in 2011 and a Sustained Grant in 2015-2017. One Heart Worldwide received a Featured Grant in 2013 and then a Sustained Grant in 2015-2017.
Fistula Foundation
Fistula Foundation is the global leader in obstetric fistula treatment, providing more surgeries to more women than any other organization, including the U.S. government and United Nations.
Fistula Foundation has 83 partners in 30 countries across Africa and South Asia. Too few hospitals offer repair surgery, which means most women must travel long distances for help, adding to the total cost of care. And a lack of trained surgeons has long been a barrier to scaling up treatment for fistula. Repair surgeries are difficult to perform and require specialized training. The goal of the Fistula Foundation Treatment Network (FFTN) model is to connect all women in all parts of a country with timely, high-quality care, building an infrastructure of treatment that will – over time and on a country-by-country basis – eradicate the suffering caused by fistula. Across the FFTN partners, the average cost for this life-changing surgery is only $619.

The FFTN model prioritizes local ownership, holistic patient care, and sustainability. Although each FFTN is adaptive to its country’s context, the core model consists of bringing together a diverse array of treatment and outreach partners to strengthen all aspects of fistula treatment across an entire country. The model integrates five core elements that lead to better, faster care: community mobilization, patient treatment, provider training and support, monitoring and evaluation, and advocacy.
FFTNs support local community health volunteers (CHVs) who educate communities about fistula and maternal healthcare and who identify women with fistula and refer them for care. FFTNs also support surgeon training and mentorship, enabling surgeons with deep experience and advanced surgical skills to cross-train and share best practices among surgical staff. FFTNs support a wide range of services, such as psychosocial counseling and job training, to help fistula survivors achieve reintegration into their communities.
Each FFTN works with local government officials to advocate for fistula education in communities and works to spread awareness of fistula through various media. By taking part in a network of holistic care, FFTN participants collaborate to address fistula on a national scale.
Learn more about Fistula Foundation
Life Challenges of the Women Served
Tanzania
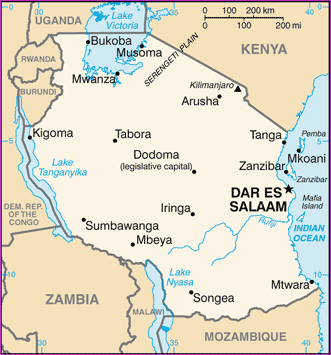 Women are among the most marginalized and underutilized Tanzanian citizens. Eighty percent of women rely on subsistence farming to feed themselves and their families. To date, about 60 percent of women live in extreme poverty. As in many other countries in the region, women make up most of the agricultural labor force, at 70 percent, yet only nine percent have sole ownership of land, only 12 percent use bank services, and women spend three times as much time as men on unpaid and domestic care work.
Women are among the most marginalized and underutilized Tanzanian citizens. Eighty percent of women rely on subsistence farming to feed themselves and their families. To date, about 60 percent of women live in extreme poverty. As in many other countries in the region, women make up most of the agricultural labor force, at 70 percent, yet only nine percent have sole ownership of land, only 12 percent use bank services, and women spend three times as much time as men on unpaid and domestic care work.
Systemic social norms make it much harder for a woman in Tanzania to have the same freedoms, education, resources, and opportunities as men. Responsibility for time-consuming household chores gives women little time for paid work. Fewer girls continue education after primary school due to lack of menstrual health supplies, early marriage, and pregnancy.
High rates of gender-based violence (GBV) continue to be a serious concern. Despite a comprehensive framework for preventing and responding to GBV, more than 20 percent of all women ages 15 – 49 have experienced physical violence in the last year – 40 percent in their lifetime. Moreover, 58 percent of women and 40 percent of men believe a husband is justified in beating his wife under certain circumstances.
Limited access to healthcare in rural Tanzania, where 70 percent of the population lives, means women are at risk of developing fistula in childbirth. Because of the vast geography of Tanzania, treatment remains out of reach for many women with fistula. Women there suffer for eight years on average before finding help. Many of these women are shunned by their communities and abandoned by their husbands. Many are unaware that their condition is treatable, and they isolate themselves out of shame.
How Our Grant Will Be Used
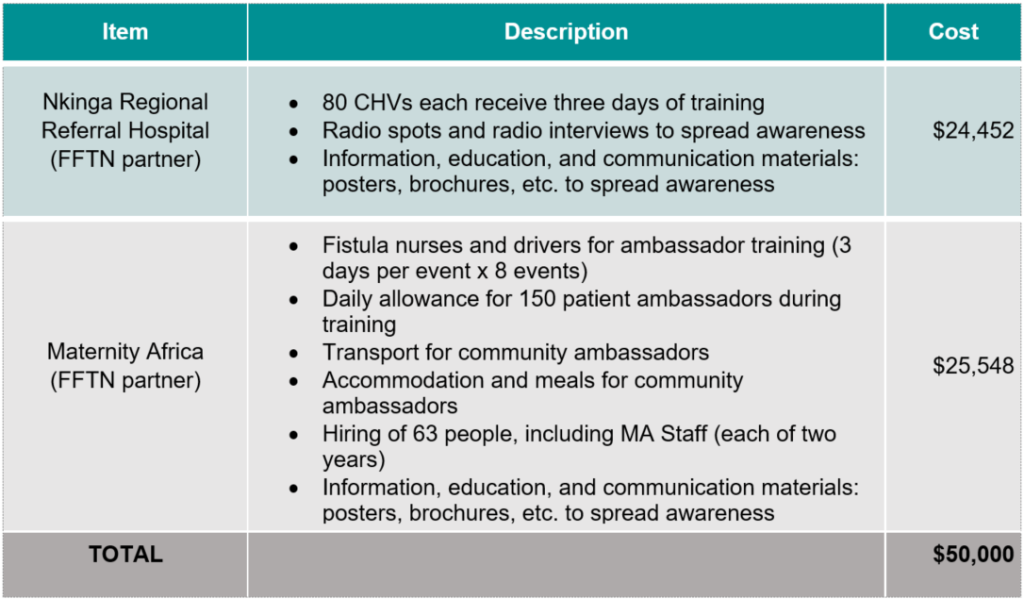
 Together Women Rise’s $50,000 Featured Grant to the Fistula Foundation is a general operations grant, supporting the important work of the foundation with two of its partners in Tanzania: Maternity Africa and Nkinga Regional Referral Hospital over two years (2024 and 2025).
Together Women Rise’s $50,000 Featured Grant to the Fistula Foundation is a general operations grant, supporting the important work of the foundation with two of its partners in Tanzania: Maternity Africa and Nkinga Regional Referral Hospital over two years (2024 and 2025).
Before the launch of FFTNs in Tanzania in 2023, Fistula Foundation had worked with each of five treatment partners in Tanzania for many years, 10 years or more in some cases. Fistula Foundation launched FFTNs in Tanzania to reach these previously unreachable women and to meet women where they are, so they can connect to the holistic set of resources available to them through the network.
Before women can seek treatment, they need to know that treatment exists. Together Women Rise’s grant will support the training of community health volunteers (CHVs) and patient ambassadors who reach women directly to raise awareness about fistula – letting them know that they are not alone and that it can be treated. Radio advertising will also be used to help spread awareness of fistula and fistula treatment options to enable the referral and treatment of women.
FFTNs in Tanzania are growing rapidly. Funds from this grant will go toward training 230 CHVs and patient ambassadors in 2024 and 2025. With outreach activities, this will enable the referral and treatment of 860 women at the two partner facilities. Across Tanzania during through 2025, Fistula Foundation aims to provide 3,053 surgeries to women with fistula, to expand its network of hospital sites by 50 percent, to train 16 surgeons, 228 nurses, and 173 other healthcare providers, and to train and build capacity among 437 CHVs.
“Fistula treatment helps to remove depression … and gives new hope. The patient leaves not as she came. She leaves changed.” —Nurse Olivia
Budget
Why We Love This Project/Organization
We love the Fistula Foundation’s work because it brings to light the cultural norms and education around younger mothers and child marriage that contribute to the prevalence of fistula while also providing prevention, awareness, and effective treatment.
Anticipated Impact & Outcomes
- 230 workers – including 150 patient ambassadors and 80 Community Health Volunteers
- Thousands of women who will no longer suffer in shame and silence from fistula
Impact Story
 Meet Violeth
Meet Violeth
Violeth (pictured here with her nurse, Olivia), a 24-year-old woman from Kongwa, Tanzania, thought that leaking urine after childbirth was normal. Her neighbors reassured her that it was part of the post-birth healing process. Violeth waited for this dark chapter to end, but several months passed, and the leaking continued.
Months later, Violeth went to a health center for a checkup. It was there that doctors recognized her symptoms, diagnosed her with fistula, and referred her to a Fistula Foundation partner in Tanzania for treatment. Violeth is now healed and dry.
One Heart Worldwide
One Heart Worldwide believes that no woman nor her infant should die during childbirth. It works to save the lives and promote the wellbeing of mothers and their newborns in underserved areas of rural Nepal.
A child born in South Asia is nine times more likely to die in their first month of life than a child born in a high-income country. For the past two decades, One Heart Worldwide has consistently demonstrated its commitment to promoting and supporting equitable access to quality health services for all through a locally- led, sustainable impact model. This model addresses – at a systemic level – the barriers to healthcare access that disproportionately affect poor women from ethnic and marginalized communities.
 In Nepal, women are too often excluded from decision-making. One Heart Worldwide’s model has been developed and refined based on evidence and guidance from those they serve, applying an approach that actively includes them and is tailored for their unique needs. Addressing issues of gender, diversity, inclusion, and compassionate communication skills are embedded in the quality of care training for rural health providers. This promotes respectful and equitable care for women, especially those in the most marginalized areas.
In Nepal, women are too often excluded from decision-making. One Heart Worldwide’s model has been developed and refined based on evidence and guidance from those they serve, applying an approach that actively includes them and is tailored for their unique needs. Addressing issues of gender, diversity, inclusion, and compassionate communication skills are embedded in the quality of care training for rural health providers. This promotes respectful and equitable care for women, especially those in the most marginalized areas.
To create a welcoming environment, One Heart Worldwide facilities include pictorial direction and visual information boards for the benefit of women who cannot read, and welcome kits with essentials for women from poor socio-economic backgrounds. Their specialized training courses also support gender equality by fostering professional development opportunities for Nepal’s Female Healthcare Volunteers and rural health providers who are often women and face professional isolation.
One Heart Worldwide’s Simulation-Based Mentorship Program supports gender equity by building the clinical and professional support needed by female health providers, which then improves equitable access to high-quality services for pregnant women in rural communities.
LEARN MORE ABOUT ONE HEART WORLDWIDE
Life Challenges of the Women Served
 Nepal
Nepal
Women in Nepal face an uphill battle due to issues of inequality and injustice. Gender discrimination and gender-based violence (GBV) are just the start. Problems are serious and widespread. Nepal’s entrenched system of patriarchy has impeded women’s ability to move outside the agricultural labor force. Though women are the main workforce in the field, they face ongoing discrimination. Seventy percent of the female population of Nepal is involved in agriculture, yet only 19 percent of the country’s land is in the name of women.
Despite the presence of many legal measures and prevention services, violence against women is a significant issue in Nepal. Women across all sectors experience high levels of GBV, including sexual harassment, assault, and domestic violence. GBV affects more than one in four women and girls in Nepal. The true scale is underreported and underestimated, since only one-third of women who experience physical or sexual violence seek help. Many victims suffer in silence due to fear of reprisal and shame. Human trafficking is another heinous form of violence in Nepal, with over 8,000 women and girls trafficked every year in the country.
Each year in Nepal, 1,500 mothers and 12,000 newborns die from preventable causes related to pregnancy or childbirth. While the Nepali government is working to improve the national healthcare system, including a focus on training skilled birth attendants (SBAs) and improving emergency obstetric care, rural districts continue to experience major gaps in healthcare coverage. Some areas lack infrastructure altogether, and many lack human resources to staff the existing facilities. Despite the Nepali government’s significant investment in maternal and newborn health (MNH) service delivery, there remain gaps in coverage within the Nepali healthcare system, particularly in rural districts.
 Growing evidence, including One Heart Worldwide’s own experience, demonstrates that many health providers lack the specialized skills to deliver quality maternal and newborn health care, and even those who participate in the official certification training for skilled birth attendants lack follow-up or opportunities to gain new information or updated techniques. Additionally, traditional training courses are largely theoretical in nature and lack opportunities for hands-on learning, resulting in a lack of confidence in applying skills or an inability to practice complex scenarios. Simulation-based approaches create rich learning environments, providing students with opportunities to practice their clinical and decision-making skills through various real-life situational experiences. Building competency to manage adverse events can positively impact patient outcomes.
Growing evidence, including One Heart Worldwide’s own experience, demonstrates that many health providers lack the specialized skills to deliver quality maternal and newborn health care, and even those who participate in the official certification training for skilled birth attendants lack follow-up or opportunities to gain new information or updated techniques. Additionally, traditional training courses are largely theoretical in nature and lack opportunities for hands-on learning, resulting in a lack of confidence in applying skills or an inability to practice complex scenarios. Simulation-based approaches create rich learning environments, providing students with opportunities to practice their clinical and decision-making skills through various real-life situational experiences. Building competency to manage adverse events can positively impact patient outcomes.
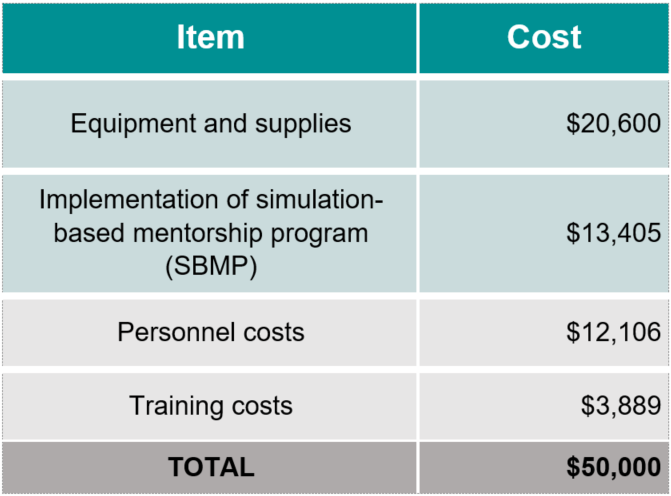
How Our Grant Will Be Used
Together Women Rise is funding a $50,000 project grant to support the expansion of the simulation-based mentorship program (SBMP) for primarily female maternal and newborn health providers in the district of Mahottari, Nepal. This will result in a stronger and more equitable health system and improved outcomes for mothers and newborns. This project builds on lessons learned from One Heart Worldwide’s previous SBMP pilot and expands the program in Mahottari district, developing a team of trainers and mentors who can deliver ongoing training sessions and provide coaching and mentoring support to rural providers in their area.
In Mahottari district, the local government often recruits newly graduated nurses with little prior exposure to maternal and newborn health service delivery and few opportunities to grow their professional capacity due to their isolated locations.
Seeking to build a team of highly trained Master Trainers and SBAs working across 13 districts of Nepal, Together Women Rise’s project will include:
- Master Trainer candidates will be selected from a pool of qualified individuals who are already working as skilled birth attendant trainers. Some Master Trainers will also come from universities, where they are faculty and lecturers on maternal and newborn health.
- To become qualified to mentor in this program, each Master Trainer will receive a seven-day certification training consisting of a five-day course on Advanced Life-Saving Skills and a two-day coaching and mentoring course. The training will include a course on the Rural Ultrasound program. As part of this combined training program, participants will not only learn the material to provide improved quality of care themselves, but they will also learn skills-transferring techniques to enable them to extend the information to all other maternal and newborn health service providers in their district over the coming years.
- The establishment of well-equipped simulation labs in district hospitals and hub facilities across program districts. These facilities will be fully equipped with practice manikins (similar to mannequins) and medical supplies to provide appropriate hands-on experience for the rural skilled birth attendants. Practice labs with neonatal manikins and “helping baby breathe” module supplies will be established at smaller health facilities to enable the skilled birth attendants to practice neonatal resuscitation.
- The implementation of regular onsite simulation-based educational sessions, during which Master Trainers assess rural skilled birth attendants and provide training and coaching. Review meetings with all program participants will allow them to share their experiences and learn from each other.
This project will also indirectly impact pregnant women and newborns from hundreds of marginalized ethnic groups. By 2030, One Heart Worldwide anticipates that its programs will impact a third (250,000) of Nepal’s pregnancies annually.
Budget
Why We Love This Program
We love this project because One Heart Worldwide is transforming maternal and neonatal healthcare across Nepal. Its programs are highly regarded by Nepal’s Ministry of Health and are being included in the national training curriculum for skilled birth attendants. Since 2010, One Heart Worldwide programs have impacted over 1 million mothers and newborns throughout 32 districts of Nepal.
Anticipated Impact & Outcomes
- Direct impact: 10 Master trainers, who will subsequently provide ongoing training and mentorship to at least 70 rural maternal and newborn health providers
- Indirect impact: 35,090 pregnant women and newborns served annually in underserved areas
From One Heart Worldwide:
“Thanks to Together Women Rise, we will be able to reach more nurses and Skilled Birth Attendants, Over the next two years, One Heart Worldwide will train 10 Master Trainers in Mahottari District, who will then go on to train and mentor 70 rural healthcare providers who work with pregnant women and their babies. The impact of these efforts is massive and profound.”
Impact Story
 Meet Nurse Manju
Meet Nurse Manju
In Udayapur District in the Koshi Province of Nepal, the One Heart Worldwide team met Nurse Manju. She began her career by completing a basic nursing education with a government institution. Following her education, Manju immediately got married and had a baby. After giving birth, she entered what is considered civil service, working for a rural health facility. However, she was unable to develop her skills. Manju said how her knowledge had reached a very low level due to lack of practice, despite her various trainings and formal education to become a nurse. Soon after, she was transferred to another health facility in Udaypurgadhi Palika (rural municipality), where her tough life as a nurse truly began. There was no transportation facility, the terrain was challenging, and the birthing center lacked any Skilled Birth Attendant.
“There were three of us nurses, and we took turns every 10 days to run the birthing center single-handedly. There was no one to guide us, and we constantly panicked even during normal birth delivery,” Manju said. She recalled how the nurses even lacked skills in diagnosing pregnant women during their antenatal care counseling at the birthing center.
“Vehicles rarely came to our village, and it was only during emergencies that off-road jeeps came this way. Every time I heard the sound of a vehicle, I was sleepless until it drove away because I thought there was a delivery case coming to us,” Manju said.
Manju lacked practical knowledge in dealing with complications. Her birthing center had several delivery cases every day, and it was tough for her to take care of all the pregnant women and mothers single-handedly. Patients were queuing up, and there was no one to help her, even to receive the newborn after delivery. At the same time, she also had to take care of the mother.
In August 2021, she had a breakthrough. The One Heart Worldwide team selected her to participate in the Simulation-Based Mentorship Program (SBMP), a hands-on simulation training program in which clinical mentors provide onsite coaching and mentoring to government nurses focused on maternal and neonatal services.
 “This training changed my life, and I consider it to be one of the most significant events in my journey as a nurse because this work is very important to me. I cannot forget how my clinical mentors Ashmita and Binita taught me step-by-step and meticulously guided me from the start,” she said.
“This training changed my life, and I consider it to be one of the most significant events in my journey as a nurse because this work is very important to me. I cannot forget how my clinical mentors Ashmita and Binita taught me step-by-step and meticulously guided me from the start,” she said.
Today, she is so confident in her knowledge that she is now also sharing what she learned with other nurses. She has no more fear of any complicated delivery cases coming to her and has been able to save countless lives. Manju’s transformation from an insecure person to a confident, skilled nurse is the kind of change One Heart Worldwide is helping to bring to maternal healthcare in Nepal.
“We need more nurses to participate in SBMP so that we can continue to update their knowledge consistently. All the lessons we learn from our mentors help us to be ready, especially in a situation when we receive any life-threatening pregnancy complications,” Manju said.
Learn More
 Country, Customs, & Cuisine
Country, Customs, & Cuisine
Proven Platter
Recipes
Source Materials
World Health Organization – Maternal Mortality
National Library of Medicine – Maternal Health
Glossary
CHV – Community health volunteer
FFTN – Fistula Foundation Treatment Network
GBV – Gender-based violence
MNH – Maternal and newborn health
SBA – Skilled birth attendant
SBMP – Simulation-Based Mentorship Program
